ACMI wants to share a series of reports from Amy Silverman on the state of services for people with serious mental illness in Arizona.
Advocates for people with serious mental illness call for improved conditions at the Arizona State Hospital, and more beds.https://azcir.org/news/2021/10/21/grievances-reforms-arizona-state-hospital/
by Amy Silverman October 21, 2021
Isaac Contreras lives alone and he says it’s making him sick.
He’s got a room and a bathroom to himself, but the luxury stops there. Contreras has spent more than a year in “administrative separation” at the Arizona State Hospital (ASH). His lawyers call it isolation.
Contreras was sent to ASH in 2017 after pleading guilty but insane to breaking his ex-girlfriend’s eye socket, cheekbone and nose, most likely during a period when he was having hallucinations associated with schizophrenia. Previously, Contreras had served a prison term for manslaughter.
As with many people with serious mental illness, Contreras’ diagnosis has changed over the years. In March 2021 it was anti-social personality disorder, intermittent explosive disorder and post traumatic stress disorder, as well as substance use disorder that’s in remission. He’s on a long list of medications.
He and his lawyers acknowledge his past, but say that a lack of proper medical care while at ASH has made Contreras worse, exacerbated during his time in administrative separation.
In his current living situation, Contreras is indoors at least 22 hours a day. Twice a day, he’s allowed to sit outside on a patio. He says that restraints are kept on his legs when he leaves his quarters. At one point, he didn’t have a table or chair; Contreras’ lawyers say that ASH officials refused to provide them, then did so after the lawyers offered to pay for the items. For a three-month stint, he was forced to eat with his hands after his spork privileges were revoked.
Holly Gieszl, a criminal defense attorney, represents Contreras along with civil lawyer Josh Mozell. Both routinely represent people in the mental health system.

“ASH didn’t give him the psych and medication support he needed to function on a daily basis,” Gieszl says. “And shortly after he was in seclusion, he started to deteriorate more.”
Mozell says that ASH has kept Contreras in isolation as retaliation for filing more than 300 grievances during the time he’s been a patient. At least two of those grievances were partially sustained, including one affirming that a staff member had physically assaulted Contreras by grabbing him in a bear hug. That employee later lost his job, in part because of the interaction with Contreras.
In another grievance filed in 2017, long before he was placed in “administrative separation,” Contreras alleged that he was kept in mechanical restraints for 14 hours, despite having been calm immediately beforehand. ASH did not sustain his grievance, so Contreras appealed the decision to the hospital.
In February 2020, ASH dismissed his concerns for a second time.
Contreras then wrote to the Arizona Health Care Cost Containment System (AHCCCS), which handles appeals. In November 2020, AHCCCS upheld part of Contreras’ grievance, noting that surveillance footage backed up his claim about being kept in restraints. AHCCCS also noted that “It does not appear that ASH conducted an additional investigation as required” given that the hospital’s second decision letter was “identical” to the first.
Other grievances were never sustained. An investigator from AHCCCS, which looks into allegations of physical and sexual abuse at ASH, confirmed that Contreras sustained a broken bone in his back after a violent incident with a staff member, but Contreras was said to have provoked the event, not the staff member.
Along with filing grievances about his living conditions and treatment by hospital staff, Contreras keeps busy by recording videos of himself talking about his situation and finding surreptitious ways to get them posted on YouTube.
“This place—if I’d known it was going to be like this, I would have told my lawyer, ‘You know what? Send me to prison,’” Contreras tells the camera.
The Arizona State Hospital is one element in the state’s mental health care system—and probably its most controversial.
While institutions like ASH are becoming a thing of the past nationwide, members of the local non-profit Association for the Chronically Mentally Ill (ACMI), and others believe there should be more beds available at the hospital; they are convinced ASH has the potential to offer therapeutic treatment that will help some of the sickest people get better and lead meaningful lives in the community.
But first, they say, reform is necessary.
Long time players in the system say oversight at ASH is inadequate because the Arizona Department of Health Services both operates and monitors the hospital.
An independent oversight committee (IOC) comprised of citizen volunteers meets monthly to discuss conditions at the state hospital. In a draft of the committee’s 2021 annual report obtained by AZCIR, members express concern that patients are complaining about being observed while toileting, without a medical reason. Guardians of patients at ASH have told the committee they are not included in the development of treatment plans. The committee noted that ASH administrators don’t attend IOC meetings.
As recently as August, committee members expressed concern over reports that patients were peeling wood and tile from the buildings at ASH and using the materials to self-harm. The IOC’s annual report included mention of “numerous reports of patients eating laminate from doors, cabinets or paneling.”
And the committee has worried about patients who claim they have been retaliated against when they complain about poor conditions. At least one advocacy organization is looking into that, too.
In response to questions from AZCIR, Arizona Department of Health Services Communications Director Steve Elliott wrote that federal privacy laws prevent him from discussing an individual patient.
“ASH uses administrative separation under limited circumstances and when necessary for the safety of patients and staff,” Elliott wrote.
In response to the Independent Oversight Committee report, Elliott wrote that the toileting concern is addressed with care.
“If a patient insists on using the restroom within 30 minutes, staff observes while providing the patient as much privacy as possible to make sure oral medication isn’t saved or disposed of. Patients on continuous observation for safety have staff present at all times, while staff make every effort possible to provide as much privacy as possible.”
He did not directly address the concerns regarding guardians not being included in treatment plans, or whether patients are removing pieces of building materials and eating them.
The 1900 Biennial Report of the Medical Superintendent of the Insane Asylum of Arizona offers far more detail about life in the state hospital than just about any modern document.
The report described two deaths in the 18-month period covered, including one by rattlesnake bite, incurred during an outing to Agua Caliente Hot Springs. The typical daily menu (including a breakfast of mush and milk, meat stew, fruit, bread, coffee and milk) is detailed, along with holiday menus and the superintendent’s Christmas gift to each patient of candy, nuts, oranges and “a useful gift.”
The population was carefully documented in a long list of patients’ occupations, including beggar, locksmith, sea captain, housewife, civil engineer and piano player. “Causes of insanity” included brain disease, masturbation, epilepsy, fright, solitary life, and “want of work.”
But for all that detail, there’s very little in the report about mental illness.
“Complete mental rest and mild physical employment have been found most efficacious in relieving cases of temporary insanity,” wrote Superintendent J. Miller, M.D.
He requested equipment and facilities that would allow for medical interventions.
“Insanity for women is commonly caused by pelvic diseases which may be remedied by surgical means,” Miller wrote, adding that the asylum was also in need of a medical library.
The hospital population was 175 in 1900.

By the late 1960s, the renamed Arizona State Hospital housed about 2,000 people with serious mental illness. But a 1970 state law requiring ASH to accept only those presenting a danger to themselves or others shrunk the number of patients to about 300, in keeping with a national trend of deinstitutionalization made possible by the introduction of medications designed to treat mental illness.
ASH was dogged by state audit findings of facilities in poor condition, overcrowding and lack of staffing in the 1990s. In a 2015 investigation, former Arizona Supreme Court Justice Ruth McGregor found dozens of instances in which Phoenix Police filed a report following a call to ASH and there was no corresponding hospital incident report documenting what happened. In addition, of more than 1,400 assault allegations, only 33 led to internal investigations and 199 to inquiries by Adult Protective Services.
The population at ASH has remained small, in part because of reforms designed to limit institutionalization.
In recent decades, some states have shuttered their psychiatric institutions as part of the goal of supporting people with mental illness in the community. Arizona stopped short of that. In the Nineties, as part of the exit criteria for the Arnold v. Sarn lawsuit that led to mandated care for people with SMI, a 55-bed limit was put in place for Maricopa County. That number was included in the 2014 settlement agreement in the case and remains the same today, despite the fact that the county’s population has more than doubled in the last 30 years since the cap was put in place.
(Here, it gets a little complicated, as ASH treats both forensic patients like Isaac Contreras, who is there because he committed a crime, and civil patients receiving court ordered treatment. The 55-bed limit applies to the civil side only.)
The debate over the 55-bed limit is heated.
Chick Arnold, the lead plaintiff in Arnold v. Sarn and a longtime mental health lawyer and advocate, signed the settlement agreement but now says he believes there should be no limit on bed count—that it’s a “clinical” decision best left to medical professionals.
Anne Ronan, a plaintiff’s attorney in Arnold v. Sarn, has a different position.
“We don’t need ASH, we never needed ASH, we don’t need two beds at ASH,” Ronan says.
“There’s nothing about the problems that the system is experiencing that gets solved by more secure housing at the state hospital.”
Carol Olson, who chairs the psychiatry department at Maricopa County’s Valleywise Health System, has a different perspective. She believes the 55-bed limit should be lifted.
She says Valleywise’s behavioral health units are overwhelmed with patients with SMI, including some who wait for more than a year for a bed at ASH. The county’s mental health units are designed for short term stays of up to 21 days.
On a given day, Valleywise fills 300-325 beds, with an ASH waiting list of a dozen or so. It’s not a large number, but it’s an important population, Olson says.
“Valleywise has become like a mini state hospital,” she says, adding that that’s unfortunate since it’s not equipped for long term stays, particularly for some of the sickest patients. Many require a private room and sometimes one-on-one staff person. There is no rehabilitation staff and not much of an outdoor area for patients.
Olson says Valleywise is very selective about whom it suggests should go to ASH.
“We don’t even consider somebody for an application to the state hospital until they have been with us for three months or longer.”
Even then, she says, ASH is often vague about why they won’t accept a patient. Olson says they will rarely accept someone who swallows foreign objects, for example, and they often won’t take a patient with a serious substance abuse disorder along with SMI, because such patients can often be stabilized in a short term facility. Olson says that’s not enough, that some need a longer stay in order to be successful and not return to a hospital setting.
Some patients simply remain at Valleywise, even when there are beds available at ASH, because state hospital administrators won’t take them.
“If we can’t safely discharge them to the community, they stay with us,” Olson says.
The health department’s Elliott did not respond directly to Olson’s charge.
“Treatment at ASH is considered ‘the highest and most restrictive’ level of care in the state,’” he wrote. “Patients are admitted because of their inability to be treated in a community facility or due to their involvement in the criminal justice system.”
Olson, who has worked at Valleywise since 1991, says Arnold v. Sarn changed things dramatically for the better by emphasizing the value of helping people with SMI thrive in the community. But now she says the pendulum has swung too far.
“Many people were placed in long-term psychiatric hospitals in the 50’s and 60’s who didn’t need to be there and nowadays do well living in the community with appropriate supports. However, there are some individuals with very severe psychiatric conditions who have only minimal or partial response to available treatments, who require a long-term stay in a locked psychiatric hospital for the safety of themselves and others and to avoid behavior which would be likely to lead to criminal charges in the community, but are not able to be admitted due to the 55-bed limit at ASH and the restrictive admission criteria there. Many of those patients instead end up in jails or prisons, which are not appropriate settings for severely mentally ill people and often make their conditions even worse.”
She adds, “I wish there would be some focus on what would be most humane for those individuals.”
In a video posted in September 2020, Isaac Contreras is wearing white sweatpants, a black tank top and shower shoes with socks. His dark hair hangs to his shoulders; he’s got a lot of tattoos, including on his face. He holds up several bottles of shampoo, soap and deodorant, as well as an electric razor, then picks up a Styrofoam container of food to demonstrate how he eats peas with his hands because he’s not allowed a spoon. He doesn’t understand why he’s given hard plastic containers, which could be used to craft weapons, but no food utensils.
He might be a man overcome by his illness, or Contreras might be the canary in the coal mine.
Either way, through his videos and grievances, he offers a window into the secret world of the Arizona State Hospital. ASH has long been a mysterious place—it’s located in the center of the city at 24th Street and Van Buren, and many people pass by the barbed wire fencing without knowing what’s inside.
In 2018, the Arizona Center for Disability Law, which is required by federal law to oversee conditions at facilities housing people with SMI, including ASH, successfully sued for unaccompanied access to patients.
The center announced that under a settlement, “ASH agreed to provide ACDL reasonable unaccompanied access to the ASH facilities and residents” and to allow the center to conduct “up to three-hour visits twice per week for the purpose of educating ASH residents about their rights and the services that ACDL provides.”
No journalist has been given a formal tour since 2015, Elliott says.
Public oversight is particularly important, critics say, because the same state agency that runs ASH is also in charge of licensing it.
AHCCCS, the state’s Medicaid agency, took on oversight of the state’s mental health system shortly after the 2014 Arnold v. Sarn settlement agreement, with one notable exception—ASH.
“Any reader in the whole world will understand why that’s bad,” says Will Humble, who served as the director of the Department of Health Services from 2009 to 2015. “The fox watching the henhouse. Everyone knows what an enormous conflict of interest that is, and up until now, no one has cared.”
Humble says that as director, he did his best to “build a firewall” between the licensing division and ASH, but believes the health department should not be monitoring a hospital it operates.
From Elliott’s written response: “It’s a common practice among states for an agency to license and operate a state hospital.”
Along with the state licensing requirements, Elliott says several other state and federal entities offer oversight, including the Centers for Medicare and Medicaid Services, adding, “ASH is one of the most regulated hospitals in Arizona.”
“The fact remains they are running and operating and regulating it themselves, and it’s not their fault, it’s the statute,” Humble says, adding that the Department of Health Services provides the staff that does the Centers for Medicare and Medicaid Services certification reviews.
Since 2018 (state records are posted for three years), ASH has had just one penalty under the health department’s enforcement actions—a $500 fine because an employee allowed two patients to be in a room alone, resulting in a sexual assault.
There was no penalty for the physical assault against Isaac Contreras, even though AHCCCS found his allegations to be true.
AZCIR reviewed incident reports from the first two weeks of January 2020. More than 175 reports were generated, including 22 marked Code Gray, which indicates combative or violent behavior.
The reports document patients hitting, kicking, biting, chasing, punching and spitting at staff, as well as attacking other patients.
From one code gray report:

It’s not unheard of for a patient to walk naked into another patient’s room. One patient reportedly masturbated during a football game. Another punched a hole in a wall when told they couldn’t have fruit late at night. During a bingo game, a patient made threats against another patient, saying, “I am going to fuck him up….I’ll go for the vital organs.”
Other reports detail patients engaging in potential acts of self-harm like tying a blanket into a knot, punching the shower wall, eating toilet paper and claiming to have eaten baby powder, shampoo and conditioner.
Three separate incident reports appear to document the same situation, in which a patient claimed to have swallowed at least 10 objects, some sharp. The reports indicated that the patient was to be observed, but there’s no information about what happened next—the spot on the incident report for “determination” is redacted, as it is on all of the incident reports released to AZCIR.
Isaac Contreras remains in isolation. It’s now been more than 15 months.
Josh Mozell says Contreras does not need to be separated from the rest of the patients at ASH. When he meets with his client, Contreras walks out to the visitor area with someone trailing him at a distance, Mozell says, which indicates to the lawyer that there’s not much reason to fear him.
Even if Contreras does exhibit violent behavior, Mozell says, there are ways to address that without isolating him. He says some patients have a one-on-one staff person or even two assigned to them.
Using nursing notes that recorded Contreras’ actions in two hour increments over the last several months, Mozell’s staff built a spreadsheet documenting that Contreras has gone weeks at a time without an issue. Legally, Mozell says, ASH is not allowed to keep him in isolation, noting that hospital officials use the term “administrative separation” although Contreras has made a crayon rubbing of the sign above his door, which says “seclusion.”
Elliott, spokesperson for the health services department, declined to comment on the specific circumstances for Contreras because of federal privacy laws.

Mozell is not the only one who’s concerned about patients kept in isolation.
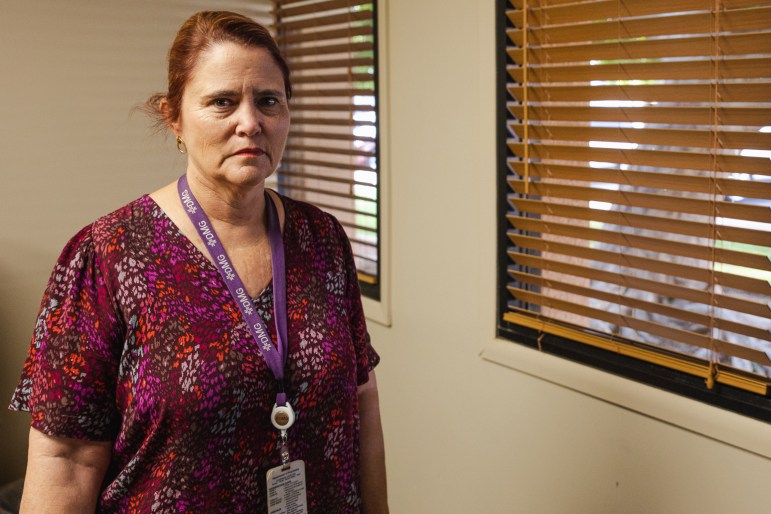
Laurie Goldstein chairs the Arizona State Hospital Independent Oversight Committee charged with monitoring conditions at ASH.
ASH isn’t all bad, Goldstein says. Her son spent a year and a half at ASH during 2013-15. She says it gave him the treatment and supervision necessary to live in the community with some support.
She’d like the hospital to do the same for others, and says she and her committee are concerned about patients kept in isolation for extended periods of time. She will not comment directly regarding Contreras, again because of privacy laws, but he has spoken before the ASH Independent Oversight Committee.
“We don’t find it particularly therapeutic if somebody was to stay in isolation their whole time and then be released,” Goldstein says.
The committee is curious about one patient’s living quarters, Goldstein says. So far, hospital administrators have refused to offer many details: “We asked to see it. They said no. We asked for pictures. They said no. We asked for dimensions. They said no.”
The committee is also worried that some patients are facing retaliation for filing grievances, which are almost never substantiated, a concern shared by the Arizona Center for Disability Law.
“The individual who actually processes these grievances, she’s the so-called patient rights advocate, but she isn’t independent. She’s an employee of ASH,” says Asim Dietrich, an attorney with the disability law center, which has a federal contract to monitor conditions at the hospital.
“Almost every ASH patient we speak to who’s filed a grievance has also received retaliation,” he says.
Since 2019, ASH has received 585 grievances from patients, according to Elliott. Of those, four were substantiated and another three were partially substantiated. AHCCCS investigates allegations of physical abuse, sexual abuse and sexual misconduct. The hospital handles the rest. The state will not release details of grievances, citing administrative code.
“I’m literally scared of getting out. Even into the unit. Not that they’re going to hurt me, but I’ve been accustomed to a small environment. I don’t understand how these people expect to help me progress if everything they’re doing is making me worse.”
ISAAC CONTRERAS
Contreras described his situation in a phone conversation with AZCIR in September. He says that being isolated is making him worse.
“Therapy was good, it helps out a lot, but that’s the only thing I get as far as treatment. All I get is my medication and any time they speak to me, it’s behind the window. I’ve never felt this hopeless before, like there’s nothing for me out there. There’s nothing.
“I’m literally scared of getting out. Even into the unit. Not that they’re going to hurt me, but I’ve been accustomed to a small environment. I don’t understand how these people expect to help me progress if everything they’re doing is making me worse.
“I have not even seen the sky, I have not seen the sun come up or go down, I have not had the luxury of that.”









You must be logged in to post a comment.